Diabetic Retinopathy
Diabetes is a disease that can affect both children and adults, and it occurs when the pancreas does not produce enough insulin or when the body is unable to process insulin properly. Insulin is the hormone responsible for regulating the level of sugar (glucose) in the blood. Patients with diabetes are more susceptible to developing eye problems such as cataracts and glaucoma. However, the effect that diabetes has on the retina—known as diabetic retinopathy— is the main threat to vision.
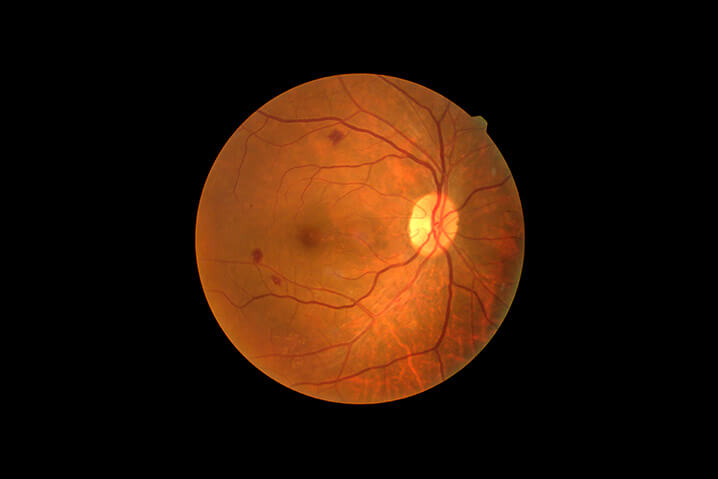
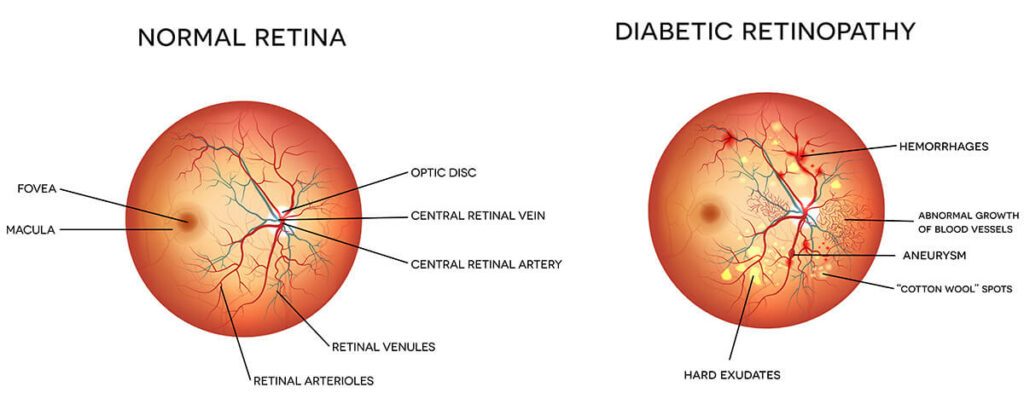
Diabetic retinopathy is when high blood sugar levels result in damage to blood vessels in the retina. The high blood sugar levels can cause these blood vessels to swell, leak, and even close, which stops blood from passing through. This condition can develop in anyone with type 1 or type 2 diabetes. The longer one has diabetes and the less controlled their blood sugar is, the more likely they are to develop diabetic retinopathy.
In the early stages of diabetic retinopathy, many people do not usually experience symptoms, although some people do notice changes in their vision like difficulty reading. In the later stages of this disease, blood vessels in the retina can start to bleed into the vitreous, which is the gel-like fluid that fills the eye. This can lead to seeing dark, floating spots or streaks that resemble cobwebs. These spots can sometimes go away on their own but without treatment, the bleeding can occur again, worsen, or lead to scarring.
As diabetic retinopathy progress, one may experience:
- Blurred vision
- Floaters (spots or dark strings floating in their line of vision)
- Fluctuating vision (vision changes from blurry to clear and vice versa)
- Dark or empty spots in their vision
- Loss of vision
There Are Two Types of Diabetic Retinopathy
Early Diabetic Retinopathy
Early Diabetic Retinopathy, often called nonproliferative diabetic retinopathy (NPDR), is the most common form of this condition. Here, new blood vessels are not growing but the blood vessels in the retina begin to weaken.
With NPDR, tiny blood vessels leak, leading to swelling of the retina, which can lead to loss of vision.
Advanced Diabetic Retinopathy
Advanced Diabetic Retinopathy, known as proliferative diabetic retinopathy is the more severe form of the condition. Here, the damaged blood vessels in the retina close off, leading to new, abnormal blood vessels growing in the retina. These new blood vessels are weak and can potentially leak in the eye’s vitreous. After some time, scar tissue from the growth of the new blood vessels can lead to the retina detaching from the back of the eye. The new blood vessels can also get in the way of the normal flow of fluid from the eye, leading to a buildup of pressure in the eyeball. This buildup of pressure can potentially damage the optic nerve, which is the nerve responsible for carrying images from the eye to the brain, which can lead to glaucoma.
Treatment greatly depends on the form of diabetic retinopathy that one has, as well as the severity of it.
- Early diabetic retinopathy may not require treatment right away but the condition must be monitored to determine when treatment is necessary. Controlled, low blood sugar levels can work to slow the progression of the condition in this early stage.
- With advanced diabetic retinopathy, immediate treatment is necessary. Potential treatment options include:
- Anti-vascular endothelial growth factor inhibitors (anti-VEGF) medications that get injected directly into the eye. These medications help to stop the growth and formation of abnormal blood vessels and decrease fluid buildup.
- Injectable steroids can be used to reduce macular swelling.
- Laser treatments can be used to reduce swelling in the retina and to make blood vessels shrink and stop leaking.
- A vitrectomy, a type of eye surgery, may be used to remove vitreous gel and blood from leaking vessels in the retina.
Diabetes & The Eye Doctors